This guide provides practical guidelines and examples for implementing the Progressive Balance Scan within PT Clinics.
Introduction
Balance tests are one of the most utilized and well-researched assessments to measure stability, asymmetry, unilateral balance, and proprioception. Neural and vestibular systems also contribute highly to the balance system, making balance assessment an important vital sign for holistic health. Balance capability has been correlated to everything from fall risk to joint pain and respiratory disease and provides a valid and reliable assessment with a variety of applications.
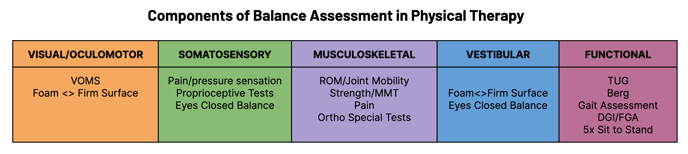
The Progressive Balance Scan is a simple assessment that guides users through a series of progressively more difficult balance challenges to assess stability, asymmetry, unilateral balance, and proprioception. The scan leverages well-established hardware (force plate) to rapidly quantify balance capabilities to expedite assessment and provide evidence-based, reliable, normative information to clinicians. It is not intended to replace but instead to augment existing clinical expertise and functional insights gleaned from other established assessments (see graphic below).
Check out our Balance Assessment Overview white paper for additional literature and references on balance testing.
General Guidelines
The Progressive Balance Scan consists of a series of progressively more difficult balance challenges and includes the following components:
- Stability - a dynamic weight shift to each side, keeping both feet on the ground to assess the most fundamental capabilities of static balance.
- Balance - a dynamic weight shift and single-leg balance to assess more advanced functional capabilities of static balance
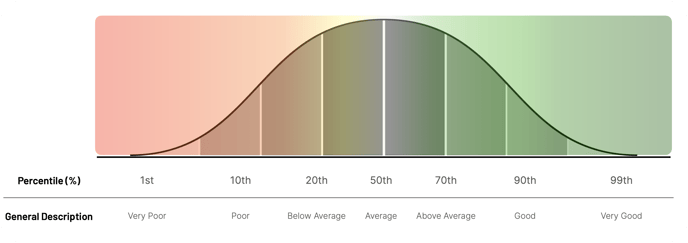
The ability to PASS through each of the different balance tasks or segments provides some initial information to the clinician about the user's balance and functional ability to complete each task. In this context, PASS indicates that the user is able to complete all segments of the scan without loss of balance (LOB) or safety concerns.

The Stability and Balance scores are derived from their Progressive Balance Scan components and represent more fundamental and advanced static balance capabilities respectively. Scores will be generated as long as the user is able to complete the segment. Higher scores indicate better balance capabilities.
Balance and Stability, and their Signature scores for each side, are all contextualized into T-score values, where 50 equals the mean or average. Higher scores indicate better balance capabilities. Anything above 50 is above average, and anything below 50 is below average.
Typical scores for the cohort or population range from 40-60, meaning the majority (~70%) of users in that group score within a 10-score range (1 standard deviation) from the average of 50. Clinicians can view scores utilizing different cohorts, which will transform scores to be relevant to a particular subpopulation. Changing the cohort ultimately compares to a different set of norms, which may alter interpretations.
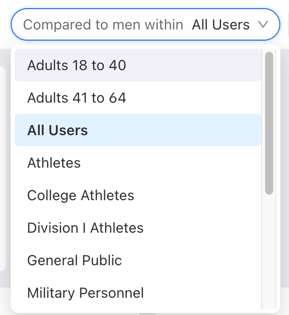
Balance and Stability are also represented as percentiles to improve interpretation. A score of 50 is equivalent to the 50th percentile (average), while a score of 60 is equivalent to the 84th percentile (above average). See the image below for a visual representation of these scores.
While a score between 50 (or 50th percentile) represents average, it is important to note that average may not always mean functional. Sparta Science Customer Success Manager Taylor Shaak, PT, DPT, OCS, explains:
Think about how we assess shoulder range of motion. We like to say that from 165-180 degrees AROM elevation is “within normal limits”. However, we still assess how our objective findings correlate with the patient’s function. A patient might have 180 degrees of elevation, but nevertheless they came to see you because they have pain every time they lift their arm. That measurement is still valuable to us because now we know maybe they can get their arm to 180 degrees, but now we need to look closer at the quality of movement and other potential pain generators to figure out what is causing their complaint.. We look at their scapulohumeral rhythm and assess synergies. We check strength, sensation, perform more special tests, etc. That range of motion measurement may be “normal”, but we still use it to help inform the rest of the assessment.
There is no “positive” or “negative” outcome with this scan– it’s giving us a snapshot in time, a baseline measure of static balance, and a reliable and objective way to then track progress in a person’s balance over time.
Tracking Balance Over Time
Regular scanning allows clinicians to track progress and patient care over time. Regular scanning intervals (such as during regular progress assessments, evaluations, and discharge) can tell the story of a patient’s progress throughout their plan of care, assisting in the therapist’s documentation and communication with providers, payors, and family members.
Practical Example
Case Report: Betty is a 75 yo female presenting to PT for functional/balance eval and tx. She has a history of two falls in the last year. Her most recent fall was 3 months ago, and she tripped over her shag carpet while walking from the kitchen to the living room and landed on her right knee. No significant past surgeries. PMHx includes DM2, osteopenia, and osteoarthritis. No injuries as a result of recent fall, though she does report some residual anterior R knee pain with walking, scale 2/10. No use of AD. All red flags have been ruled out and you’re now ready to initiate a standing balance evaluation.
Rationale: Betty is full weight bearing, does not use an AD, and is able to stand and ambulate independently. She does not present with cognitive deficits or excessive fear. It is clinically appropriate to initiate a standing balance assessment, though you are unsure of her full functional capabilities.
Reference:
- PASS: Pt is able to complete all elements of scan without LOB, safety concerns
- FAIL: Scan is stopped by therapist or patient due to safety concerns, pain, LOB, etc.
* This is a use case example outline to help physical therapists contextualize the workflow implementation of the Progressive Balance Scan. Examples of evaluation rationale and assessment choices are used for therapist understanding and contextualization of flow only and are not meant to replace or substitute for the clinician’s expertise or reasoning in developing his/her POC.
Additional Tips
There are some instances in which the scan results may not line up with what you see clinically, and that can create confusion for both you and the patient. Like most of our special tests, insignificant findings are usually just a sign to dive deeper or refine our differential diagnoses.
Key Takeaways
- The Balance score is an aggregate of metrics that capture an individual’s static balance capabilities on a firm surface with eyes open at one moment in time. These are objective, evidence-based insights.
- It’s important for us and our patients to understand what “normal” or “average” is, but that doesn’t mean that’s always what’s functional for that specific patient. These results are meant to guide your clinical judgment, not replace it.
- This is meant to be an objective tool to help you reliably assess an individual’s balance or movement health in a way that is standardized, accurate, and easily repeatable.
